The Transformative Care Model

Transformative care brings together evidence-based treatments with sophisticated self-management training to reduce risk factors, enhance protective factors while improving outcomes and patient satisfaction. Transformative integrates treatments from health care professionals, health coaches, patients, and their support network to improve outcomes and prevent chronic pain. Clinical trials have found that patients who are engaged in self-care have significantly better outcomes than any biomedical treatments alone. There is a need to train health care professionals to implement this new model of health care to not only transform patients’ lives but also the health care system.
Implementing transformative care:
- Personalized assessments to identify risk and protective factors
- Self-management training to reduce risk and enhance protective factors
- Evidence-based bio-medical treatments
- Interdisciplinary integrative team with a health coach to support patient training
- Innovative bundled reimbursement models
- New paradigms of care
New Paradigm of Care
A human systems approach provides a broader understanding of the role of diverse lifestyle risk factors and protective factors in perpetuating chronic pain through recursive feedback cyles that increase periperhal and central sensitization. Implementation strategies including developing whole patient problem lists, identifying all risk and protective factors, integrative team care with a health coach, shifting health care paradigms, and use of health information technology will shift the balance of care from one of a passive patient to an empowered, engaged, and well-trained patient to not only prevent chronic pain but also enhance health and wellness. Ultimately, this will not only improve the quality of care, pain, and functional outcomes, but also significantly reduce health care costs.
New concepts of Healthcare
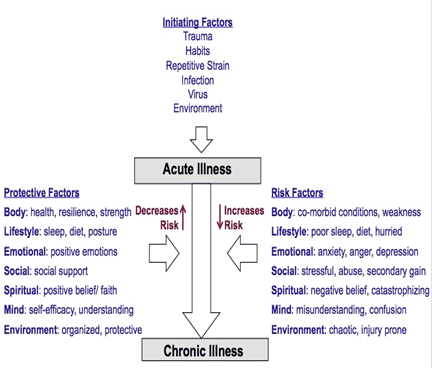
Human are complex, multi-dimensional, and dynamic and live within an ever-changing physical and social environment. Yet, our traditional bio-medical model is based on a scientific paradigm that is uni-dimensional, reductionistic, and inflexible that is based primarily on understanding the underlying pathophysiology. Health care professionals tend to see what they treat and treat what they see. If they see only the pathophysiology, they do not recognize and understand the complex risk and protective factors that interact and play a powerful role in the onset, perpetuation, and progression of an illness. As a result, success of treatment is often compromised by limited approaches that only address part of the problem. When treatment approaches are limited, outcomes are limited. This explains why systematic reviews of efficacy of nearly every bio-medical treatment for chronic illnesses have shown that even with the most efficacious treatments, they improve outcomes by only 10 to 20% above placebo. Patients have more control over the outcomes of their illness than any treatment provided by clinicians. Thus, when evidence-based bio-medical treatments are combined with robust self-management training within a transformative care model, they have transform the patient from one of illness to health and wellness.
While distinct pathophysiological mechanisms occur in all chronic conditions, understanding and changing the multitude of factors that play a role in the onset, perpetuation, and progression of the illness is the key to successful management. This is the basis behind transformative care. All physical illnesses are intertwined with the person’s thoughts, attitudes, behaviors, emotions, and environments. As Sir William Osler, “It is much more important to know what sort of a patient has a disease than what sort of disease a patient has.”
Engaging Health Professionals

Health care professionals need to be trained transformative care to understand this new epistemology and implement robust self-management training with the best and safest evidence-based treatments. In the process, patients become active participants in their own pursuit of health and well-being to achieve optimal whole person health not only for each episode of care but throughout their lifetimes. The Chronic Pain Research Network provides health professionals strategies to facilitate implementation of transformative care for chronic pain conditions. The Network will use innovative health information networking technology, on-line training, workshops, and seminars.
 |
Achieve the Institute for Health Care Improvement’s Triple Aim of improving the health care system by achieving goals of improving the patient’s experience of care, improving the health of the patient, and reducing the cost of health care. However, those who benefit the most may not only be the patients receive care but the health professionals providing it. |
 |

