New Approach to Chronic Pain is Needed
To improve the chronic pain problem, the focus must be on prevention and early intervention of chronic pain. To do so, we need a broader conceptual model, shifting paradigms of care, new strategies for care delivery, and better ways to train patients. A human systems approach provides a broader understanding of the role of diverse lifestyle risk factors and protective factors in perpetuating chronic pain through recursive feedback cycles that increase peripheral and central sensitization.
Human Systems Approach

A broader conceptual basis is also required to improve chronic pain among the vast majority of patients. Many concepts are included in human systems approach including risk and protective factors in the seven realms, neuro-plasticity, positive psychology, cybernetics, chaos theory, and cognitive-behavioral approaches. Each bring a new understanding of the balance between health and illness as presented in Table 1 Human systems theory (HST) stems from research in general system theory and originated in ecology out of the need to explain the inter-relatedness of organisms in ecosystems. While conventional biological theories view the subject as a single entity, HST views a person as a whole with an inter-relationship between the sub parts of their life. These sub parts are not “static" but rather are dynamic, evolving, and interrelated processes.
| Table 1. The broad conceptual framework of human systems approach to care | ||
|---|---|---|
| Human systems | “See the big picture” | Risk factors and protective factors in the seven realms of life including body, lifestyle, emotions, society, spirit, mind, and physical environment determine what is the balance between health and illness |
| Neuroplasticity | “We are what we think?” | The brain is constantly changing its structure, synapses, and efficiency throughout our lifetime due to environmental, social, and lifestyle factors that can enhance intelligence, physical performance, insight, and happiness as well as reduce chronic pain and illness. |
| Cybernetics | “What goes around comes around” | Each element of a system generates a change, which causes positive or negative feedback to the entire system and leads to 1st order reactive change, 2nd revelation change, or 3rd order transformative change. |
| Chaos Theory | “It’s the little things every day that matter most.” | Small differences in initial conditions may yield widely diverging outcomes within dynamic systems like humans. Thus, the influence of multiple small risk and protective factors can play a big role in shifting the balance between health and illness. |
| Cognitive-Behavioral Theory | "We are what we repeatedly do.” | Specific goal-oriented and repeated positive actions can improve dysfunctional emotions, behaviors, and cognitions and help restore health and wellness. |
| Positive psychology | “We become what we think.” | By training our brains to focus on the positive thoughts and emotions and being mindful of them, the potential to be healthy and well is enhanced. |
As illustrated in Table 2, the practical application of HST to patient care in comparison to the bio-medical model includes the use of personalized assessments, whole person problem lists, identifying risk and protective factors, integrative team care, use of medical coaches, shifting health care paradigms, and use of health information technology provide innovative strategies to implement trans formative care. Care is shifted from one of a passive patient receiving a treatments to an empowered, engaged, and well-trained patient focusing on both prevent and alleviating chronic pain but also enhancing health and wellness. Since patients expect to have a passive role in care, specific paradigms need to be conveyed to the patient as illustrated in Table 3 to shift the responsibility for success from the clinician to the patient. Ultimately, this paradigm shift will not only improve the quality of care, pain, and functional outcomes, but also significantly reduce health care costs, achieving the Institute for Health Care Improvement’s triple aim.
| Table 2. Comparison of the traditional bio-medical model and a human systems model | ||
|---|---|---|
| Concept | Bio-medical Model | Human Systems Model |
| Conceptual basis | Reductionistic, mechanistic, inflexible | Holistic, fluid, flexible |
| Application of scientific methods | Relies on objective physical measures, single brief interventions, and randomized controlled trials | Relies on objective and subjective measures, multiple interventions over longer periods, and pragmatic clinical trials |
| Etiology | Pathophysiologic etiology based on single static etiology (e.g. infectious agent, structural change, cancer) | Multifactoral dynamic etiology of chronic illness (e.g. risk and protective factors influence on physical structures) |
| Problem list | Identify chief complaint and diagnosis in the physical or psychiatric realm | Identify chief complaints, diagnosis, and contributing factors in seven realms of life |
| Treatment strategy | Unidimensional that encourages single sequential treatments | Multi-dimensional that integrates multiple interventions with self-management |
| Providers | Single clinician providing single intervention that is easy to implement. May lead to fragmented approaches | Interdisciplinary integrative team of clinicians that address multiple levels of contributing factors with multiple interventions and thus, more complex to implement |
| Reimbursement | Well supported by delivery system and health care economic model which rewards procedures over process | Mostly not supported by current delivery system and health care economic system |
| Outcomes | Good outcomes with acute conditions Poor outcomes with chronic illness due fragmentation of multiple single treatments. | Good outcomes with chronic illness due to use of trans formative care model with self-management, bio-medical interventions, and a team approach |
Transformative Care The Institute of Medicine’s (IOM) 2011 monograph, “Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education and Research,” strongly supports the need for prevention and self-management by stating that “health care provider organizations should take the lead in developing educational approaches for people with pain and their families that promote and enable self-management.”1 However, these changes require transformation of the health care system that would be a challenge for even the most innovative and revolutionary health care professional. Clinical trials and systematic reviews have found the outcomes of self-management strategies that activate the patient through exercise and cognitive and behavioral changes equal or better than passive treatments.26-34 However, when self-management is combined with these evidenced-based bio-medical treatments, the outcomes can be dramatically improved while also reducing the patient’s dependency on the health care system.35-40
A transformative care model accomplishes this by integrating personalized assessments, robust self-management training, and evidence-based bio-medical treatments to help patients reduce risk factors, enhance protective factors, and reverse the perpetuation of chronic pain. This can only occur through an interdisciplinary integrative team-approach to clinical practice that can be sustained through innovative bundled reimbursement models. The balance between risk factors and protective factors determine whether an acute problem progresses to chronic pain or not as illustrated in the Figure. Thus, it is paramount in the clinical application of transformative care to identify and reduce risk factors for chronic pain and train the patients in improving protective factors.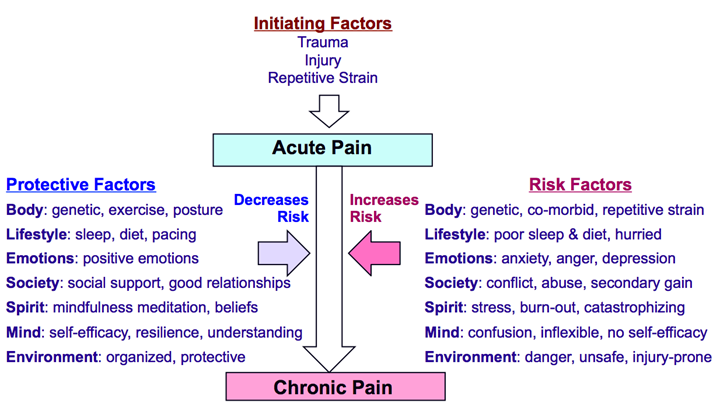
| Table 3. The new paradigms associated with trans formative care and a human system’s approach | |
|---|---|
| New paradigm | Statement that shifts to the new paradigm |
| Understand the whole patient | We will help you identify all diagnoses, risk factors, and protective factors associated with your condition |
| Every patient is complex | Every patient is complex. There are multiple pre-conditions, conditions, and many inter-related contributing factors that may initiate, result from, increase risk, decrease risk, and need to be addressed as part of management strategy |
| Self responsibility | You have more influence on the problem than any treatment provided. You need to take ownership. |
| Self-care | You will need to make daily changes in order to improve your condition |
| Education and training | Health care providers will need to teach you how to make these changes. |
| Long-term change | Change only occurs over time and it may take months for the changes to have a large impact on reducing pain and symptoms. |
| Strong provider-patient partnerships | Health professionals will support you as you make the changes. |
| Personal motivation | Will you be able to make the changes need? |
| Social Support | You may need help to make these changes. |
| Fluctuation of progress | Expect ups and downs during the recovery process. |

